Pioneering detailed lung MRI scans without radiation
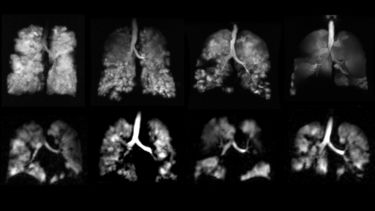
Scientists at the University of Sheffield have developed a novel type of MRI scan that produces unique images of the lungs. The safe scan uses inhaled hyperpolarised xenon gas to pick up on lung abnormalities previously undetected with routine tests.

The Pulmonary, Lung and Respiratory Imaging Sheffield (POLARIS) research group led by Jim Wild, Professor of Magnetic Resonance Physics and Director of the INSIGNEO institute for in silico medicine at the University of Sheffield is at the forefront of developing this novel method of MRI technology. Using this sensitive method, the group is pioneering new research and translating it to clinical practice across the NHS.
These groundbreaking xenon functional imaging technologies used in conjunction with structural proton MRI have helped clinicians identify early signs of lung disease, for example in children with Cystic Fibrosis and adults with severe asthma, without using radiation.
The methods are very sensitive to picking up limitations of gas exchange in the lungs. Sheffield are leading studies with xenon MRI to improve our understanding of post Covid lung disease, interstitial lung disease (scarring of the lungs) and pulmonary vascular disease (any condition that affects the blood vessels within the lungs). To date, this research with multi-nuclear MRI has helped define NHS practice in the diagnosis and management of patients from the Sheffield Interstitial Lung Disease and Pulmonary Vascular Disease clinics.
The new lung MRI scanning technology, which is a collaboration between the University of Sheffield and GE Healthcare, is one of 19 initiatives receiving part of £149 million in funding by the Engineering and Physical Sciences Research Council (EPSRC), UKRI’s Biotechnology and Biological Sciences Research Council (BBSRC) and Medical Research Council (MRC).
Respiratory disease affects one in five people in the UK, creating a massive burden on healthcare which costs the NHS more than £6 billion per year. This partnership hopes to make advanced functional imaging more accessible to respiratory medicine.
But how does this novel MRI scan work?
Understanding body scans
Typically magnetic resonance imaging (MRI) and computerised tomography (CT) are used to provide images of tissues in the body to help diagnose internal problems.
An MRI scan is a non-invasive technology that uses strong magnetic fields to magnetise the protons in water and fat tissues in the body. Radio-frequency waves shift these protons to create a signal and radio frequency coils encode these signals by time varying magnetic fields to create 3D images of the body.
A CT scan uses X-ray detectors to create images of slices of the body. As well as being used to quickly examine internal injuries from trauma, it can also be used to visualise nearly all parts of the body. As CT scans use radiation however, they cannot be used repeatedly in a short period of time due to a heightened risk of harming the patient, this becomes a particular issue in children.
Where conventional proton MRI and CT scans fall short, is their ability to provide insight into the function of the lungs at the physiological coalface - the interface between the alveoli and capillaries. A new approach to imaging was needed that is safe, repeatable and accurate. This is what the POLARIS team have delivered.
Sheffield’s solution to safe, clearer imagery
Developed at the University of Sheffield, the POLARIS technology uses inhaled Hyperpolarised Xenon gas in combination with MRI scanners (retuned to the xenon frequency) to provide clear images of internal organs and to measure their function.
The gas is magnetised (or ‘hyperpolarised’) outside of the scanner so that the majority of the Xenon atoms are aligned. This creates a strong signal that can be picked up by MRI scans from relatively low concentrations of the inhaled gas. The gas is safe to inhale, soluble and gets taken up to the brain by the blood in the lungs.
As well as providing novel information on gas exchange in the lungs, it is the first MRI method currently available to provide direct visualisation of gas exchange in the brain. Researchers at Sheffield were the first to demonstrate this high quality xenon brain MRI.
“Patients are asked to inhale the Xenon gas, hold their breath for a few seconds while the scanner collects the images and then breathe the gas away” explains Professor Jim Wild.
This technology is exquisitely sensitive, safe (even for children and infants), and is being used in a variety of ways such as measuring the efficacy of novel treatments for lung diseases in collaboration with pharmaceutical companies. So far, the team at POLARIS have collaborated with AstraZenaca, Boehringer-Ingelheim, GlaxoSmithKline and Novartis. The images generated are also used as the basis for computer models of lung microstructure and physiology, and the research is central to the themes of the INSIGNEO institute, spanning advanced biomedical imaging, novel device technology and computational modelling.
The scan takes just a few minutes and, as it does not require radiation exposure, it can be repeated over time to see changes in the lungs with disease progression and in response to treatment.
Professor Jim Wild
Professor of Magnetic Resonance Physics at the University of Sheffield
The methodology developed by POLARIS is approved by the MHRA in the UK and is being used in NHS patient pathways and to evaluate new treatments by Pharma in the UK and EU.
Supporting children with Cystic Fibrosis
Cystic Fibrosis (CF) is a progressive genetic disorder that causes severe damage to internal organs such as the lungs and digestive system. The disorder causes a build-up of thick mucus, blocking ducts and tubes in internal organs such as the lungs, bowel, and pancreas. Typical symptoms include a persistent cough, wheezing and frequent lung infections. Over 10,000 people live with CF in the UK.
Doctors usually evaluate the progress of the condition using a chest X-ray or a CT scan. However, frequent CT scans involve high exposure to radiation which poses high risks to patients, especially for children.
Using this novel MRI method, POLARIS uncovered details in lung ventilation difficulties that were not picked up in previous CT scans without using any radiation.
This MRI method is now being used for the detection of early functional lung disease as an alternative to a chest X-ray or CT scans by the Sheffield Children’s Hospital CF Clinic. This service is novel to the UK.
Understanding post Covid lung disease
Many people who have had Covid developed acute lung injury. POLARIS have led the way in the UK with this technology to help understand how the function of the lungs is impaired and why some people recover and others seem to have persistent breathlessness.
They have created a national platform for the use of this technology in two large collaborative studies: the UKILD study and the EXPLAIN study.
Sheffield’s hyperpolarised xenon MRI scans are at the core of the EXPLAIN study.
This study involves teams at Sheffield, Oxford, Cardiff and Manchester to investigate lung damage in Long Covid patients who have not been hospitalised but continue to experience breathlessness. The initial results from the pilot showed that there is a ‘significantly impaired gas transfer’ from the lungs to the bloodstream in Long Covid patients although other conventional tests were normal.
Imaging of the human brain
Once the Xenon-129 gas has been inhaled into the lungs, it also safely dissolves into the pulmonary blood stream and transported to organs such as the brain and kidneys. However, only a small fraction (less than 5%) of the gas travels from the lungs to the brain, which has been difficult to pick up on in MRI scans in the past.
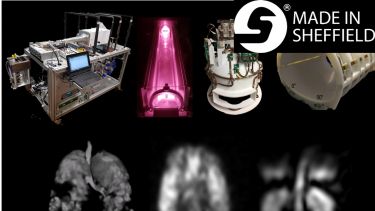
POLARIS have developed new, highly-sensitive equipment that has allowed for the direct, clear imaging of the MRI gas to be picked up as it travels to the brain tissue.
Looking ahead
Their research into this novel MRI scanning has been used to perform the world’s first clinical diagnostic scanning with this technology in Sheffield in partnership with Sheffield Teaching Hospitals and Sheffield Childrens Hospital.
The POLARIS group are now focusing on making the technology more clinically accessible by supporting new clinical sites around the world with gas polarisers and the methods needed to make standard clinical scanners pick up the xenon signals. The team are also working closely with GE Healthcare to help make lung MRI techniques feature as a clinical product on their MRI scanners.
The revolutionary MRI scans will benefit from part of a £149 million investment to bring UK business and academics together to accelerate cutting edge research.
“This new £2.7 million funding and industry collaboration with GE Healthcare will help us to develop and integrate computer hardware and software making it possible to use hyperpolarised xenon technology on existing MRI systems and further research high-quality imaging at low-field strengths. This will not only save money but it will also make the revolutionary imaging available to more patients and groundbreaking clinical research" says Professor Jim Wild.
Written by Alina Moore, Research Communications Coordinator
Some examples of lung applications:
General use in the NHS for clinical lung imaging
Lung MRI with hyperpolarised gases: current & future clinical perspectives.
Stewart NJ, Smith LJ, Chan HF, Eaden JA, Rajaram S, Swift AJ, Weatherley ND, Biancardi A, Collier GJ, Hughes D, Klafkowski G, Johns CS, West N, Ugonna K, Bianchi SM, Lawson R, Sabroe I, Marshall H, Wild JM.Br J Radiol. 2022 Apr 1;95(1132):20210207. doi: 10.1259/bjr.20210207. Epub 2021 Jun 9.
Covid
Cystic Fibrosis
The assessment of short and long term changes in lung function in CF using 129Xe MRI.
Smith LJ, Horsley A, Bray J, Hughes PJC, Biancardi A, Norquay G, Wildman M, West N, Marshall H, Wild JM.Eur Respir J. 2020 Jul 6:2000441. doi: 10.1183/13993003.00441-2020.
Asthma
Xenon ventilation MRI in difficult asthma: initial experience in a clinical setting.
Mussell GT, Marshall H, Smith LJ, Biancardi AM, Hughes PJC, Capener DJ, Bray J, Swift AJ, Rajaram S, Condliffe AM, Collier GJ, Johns CS, Weatherley ND, Wild JM, Sabroe I.ERJ Open Res. 2021 Sep 27;7(3):00785-2020. doi: 10.1183/23120541.00785-2020.
Xenon in the brain
Assessment of brain perfusion using hyperpolarized 129 Xe MRI in a subject with established stroke.
Rao MR, Norquay G, Stewart NJ, Hoggard N, Griffiths PD, Wild JM.J Magn Reson Imaging. 2019 Sep;50(3):1002-1004. doi: 10.1002/jmri.26686. Epub 2019 Feb 18.
The technology
^{129}Xe-Rb Spin-Exchange Optical Pumping with High Photon Efficiency.
Norquay G, Collier GJ, Rao M, Stewart NJ, Wild JM.Phys Rev Lett. 2018 Oct 12;121(15):153201. doi: 10.1103/PhysRevLett.121.153201.
Norquay G, Collier GJ, Rodgers OI, Gill AB, Screaton NJ, Wild J.Br J Radiol. 2022 Apr 1;95(1132):20210872. doi: 10.1259/bjr.20210872
Collier GJ, Eaden JA, Hughes PJC, Bianchi SM, Stewart NJ, Weatherley ND, Norquay G, Schulte RF, Wild JM.Magn Reson Med. 2021 May;85(5):2622-2633. doi: 10.1002/mrm.28609. Epub 2020 Nov 30.PMID: 33252157
Stewart NJ, Norquay G, Griffiths PD, Wild JM.Magn Reson Med. 2015 Aug;74(2):346-52. doi: 10.1002/mrm.25732. Epub 2015 Apr 27.