Sheffield Pain Network
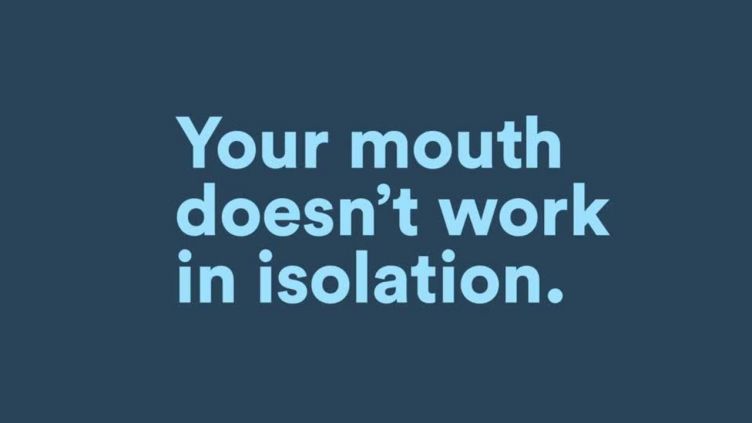
Pain is a complex multidimensional experience, affecting a wide range of people. We are bringing together experts from across the University of Sheffield to improve the understanding and treatment of pain.
Impact and latest research
Trigeminal nerve repair
This video will guide you through the causes, symptoms and treatment options for trigeminal nerve damage, highlighting research at the University of Sheffield.
Contact us
Please get in touch if you have a research idea or would like to collaborate with us.
Professor Fiona Boissonade, Network Director: f.boissonade@sheffield.ac.uk